
Ms Sharon (Ling Zhi) Heng
MBBS, PhD, FRCOphth, FHEA
Consultant Ophthalmic Surgeon
What is Retina Vein Occlusion?
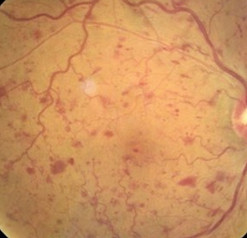
Retina vein occlusion or also known as retinal vascular occlusion is a known cause of sudden painless loss of vision. This happens usually in older patients and is caused by a blockage in the veins of the retina , in most cases associated with hypertension.
There are two main types of retina vein occlusion:
a) Branch retinal vein occlusion (BRVO) which is blockage of one of the retina veins (60-70% of patients diagnosed with vein occlusion) and
b) Central retinal vein occlusion (CRVO), which is blockage of the main retina vein where blood flows out of the retina.
Getting treatment early can reduce the chance of vision loss.
What are the Symptoms of Retina Vein Occlusion?
Most patients are asymptomatic and are diagnosed on routine ophthalmic retina checks, but some may present with painless loss of vision.
What Causes Retina Vein Occlusion
A blockage(usually a blood clot) forms in the vein, causing obstruction to the retina blood flow. There are some known systemic associations with retina vein occlusion which include:
-
Hypertension or high blood pressure
-
Hypercholesterolemia or high cholesterol
-
Diabetes
Retina vein occlusion has been found to be more common in patients with diabetes. Diabetic screening and optimise diabetic control will help to pick up symptomless vein occlusion and prevent recurrences. -
Glaucoma or increased intraocular pressure- increase in pressure in the eye.
There is a known association between glaucoma and retina vein occlusion. Anti-glaucoma treatment to reduce eye pressure to an adequate level is key to preserving vision and prevent further recurrences of vein occlusion
In a smaller cohort of patients, especially patients of a younger age group or less than 50, further detailed investigations are usually performed to rule out causes of vein occlusion. These may include tests to rule out causes such as retina inflammation (uveitis) or certain rare blood disorders that may cause hyper-coagulation of blood in patients.
How is Retina Vein Occlusion Diagnosed?
As the majority of cases are asymptomatic, many cases are diagnosed as incidental retina checks or screening. This usually involves clinical examination, fundal examination of the retina, wide field imaging and optical coherence tomography scans (to rule out macular oedema or fluid in the eye).
In some cases, we will need to perform angiography tests such as fluorescein angiography to assess for retina ischemia and abnormal new vessels.
If a patient has painless loss of vision, please do see an ophthalmologist on an urgent basis for a review and imaging to diagnose the disease and assess for any complications that may result from it.

How is Retina Vein Occlusion Treated
Treatment of retina vein occlusion is dependent on the sequelae of the disease.
Retina vein occlusion may cause fluid in the eye or otherwise known as macular oedema. This will cause vision to be blurred or distorted. Another known sequelae is abnormal new blood vessel growth or otherwise known as neovascularisation. This can be asymptomatic, or in advanced stages, the new vessels may grow in the anterior segment and cause neovascular glaucoma where patients present with a painful eye.
Treatment for Fluid in the Eye (Macular Oedema)
Macular fluid build up in the macular which is the centre of the retina is caused by damaged blood vessels which leaks fluid. There are different treatment modalities which include the following:
Anti-VEGF Intravitreal Injection
The injections are usually given monthly during the loading dose phase (usually 3 loading doses) after which, depending on treatment response, stop or be or given on extended intervals until stabilisation of disease activity.
Earlier treatment has been shown to improve visual outcomes.
Steroids
Steroids are given as an eye injection either in the form of a one off injection or an implant which lasts for 4-6 months into the eye.
Approximately 50% of patients treated with anti-VEGF injections experience significant improvements in vision of more than 3 lines on the vision chart on measurement. Steroid implants have similar results. Unfortunately, approximately 20-30% experience no improvement in vision following injection treatment regardless of modality
Further information on how eye injections are given or risks of treatment can be found https://www.retina-eye.co.uk/intravitreal-anti-vegf-injections

Macular Laser
Depending on the fluid profile, macular laser may be a treatment option to consider in selected groups of patients. During the consultation, Ms Heng will discuss your prognosis depending on your disease profile and imaging biomarkers to determine the best course of treatment for you.
B. Treating Neovascularisation or Abnormal Growth of New Vessels
Unfortunately, 1 in 5 patients with retinal vein occlusions will develop abnormal blood vessels either in the retina or the front of the eye at the iris. These abnormal blood vessels can bleed (vitreous haemorrhage) or cause an increase in eye pressure, leading to further loss of vision and unfortunately, pain in some cases.
Treatment is usually with either laser to the periphery of the retina, also known as pan retina photocoagulation (PRP) or antivegf therapy. Treatment in these stages are aimed at stabilizing the retina and prevent worsening of vision. It will not improve vision.
Usually, patients are monitored on a 4- 6 weekly basis for the first 6 months then over an extended interval for minimum of 2 years to monitor for sequelae of the disease.